“Innovation Gives You Hope”

In 2011, when Mary Jo Rogers learned she had Stage 3 melanoma, William Sharfman, MD, presented her a couple of options. The traditional treatment promised unpleasant side effects and was proven effective in about 10 percent of melanoma patients. Enrolling in a clinical trial for a new immunotherapy treatment carried the risk of the unknown but also the potential to reverse her cancer’s spread with less severe side effects.
Rogers and her husband, Brian, chose the latter path, and by 2014, her tumors had all but disappeared. Grateful for Sharfman’s guidance through two clinical trials, the Rogers focused their philanthropy on making a difference for other melanoma patients. They made a gift to endow a professorship for Sharfman — the first named chair in the Bloomberg-Kimmel Institute for Cancer Immunotherapy — which was supported by the State of Maryland as well.
By investing in the institute through the professorship and an additional gift — a research endowment to support immunotherapeutic discovery in melanoma — the Rogers are helping to make immunotherapy a viable avenue for more cancer patients.
“Innovation gives you hope. The worst thing that could happen is that there is no more innovation, and there is no more hope,” Brian says. “A large part of our experience was to hang in there as long as we could, hoping for science to come up with a new treatment. We were very lucky that it did.”
“We’re so grateful for what Dr. Sharfman and others were able to do for me,” says Mary Jo, now an advocate for melanoma patients and survivors. “This is one way we are able to pay it back.”
"It Gives You a Spark to Keep Going"
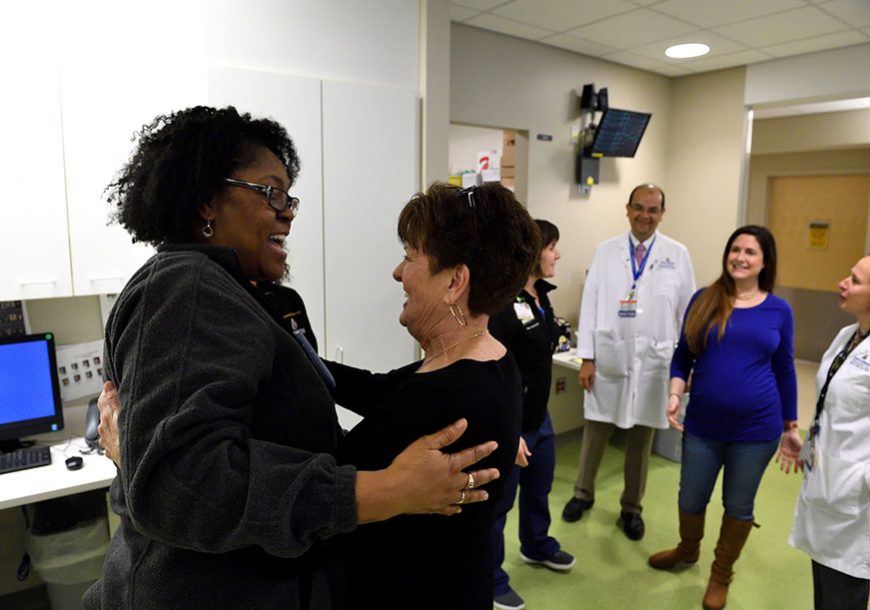
For much of the past decade, Anna Sowers, MBA (Bus ’09), Kim Good, and Taylor Harris have gathered once a year at Johns Hopkins Hospital to mark one of the hardest moments of their lives. In March 2008, Zach Sowers — Anna’s husband, Kim’s son, and Taylor’s brother — died, having spent months in a coma after a mugging outside his home in Baltimore’s Canton neighborhood.
The women’s annual visits to the Neurosciences Critical Care Unit (NCCU) began as a way to thank the nurses and doctors who cared for Zach; Good would bake and bring cookies to the units both in East Baltimore and at Johns Hopkins Bayview Medical Center.
“It keeps Zach’s name alive,” Good says. “When we go see and meet everyone each March, it gives you a spark to keep going.”
In recent years, they’ve also met with young researchers whose work is supported by the Zach Sowers Brain Trauma Research Fund. The fund — which began as a way to help the family pay for Zach’s medical bills — has grown into a valuable resource for physician-scientists in the Department of Anesthesiology and Critical Care Medicine.
“It’s growing harder for anyone to have access to federal funding, especially as junior faculty,” says Jose Suarez, a professor of neurology and the current director of neurosciences critical care at Hopkins. “The Sowers Fund allows us to have an internal grant opportunity, assign funds to at least two fellows at a time, and give them a kickstart on their research and maybe bigger funding in the future.”
Sowers, Good, and Harris have raised money for the fund — which currently totals more than $88,000 from more than 400 donors — through a variety of annual events.
“If this fund can help one person, or two, or three — through research, maybe, someone would have a better prognosis in Zach’s situation than he did — it will be worth it,” Harris says.
Transforming Stroke Diagnosis and Treatment

Sheikh Khalifa Stroke Institute, funded by gift from the United Arab Emirates, brings together experts in neurology, rehabilitation, biomedical engineering, and patient safety to address a significant global health challenge
Funded by a $50 million gift from the UAE, the Sheikh Khalifa Stroke Institute will enable top clinician-scientists at Johns Hopkins to build on their pioneering work in neurology and neurosurgery, leveraging advances in biomedical engineering, artificial intelligence, and precision medicine to better diagnose, treat, and restore function to stroke patients. The gift is believed to be the largest ever for a stroke-specific initiative.
The new institute boasts locations in Baltimore and Abu Dhabi.
“We are grateful for the UAE’s gift, which enables us to leverage our considerable strengths in neurology, physical medicine, and rehabilitation—in combination with our expertise in biomedical engineering and patient safety—to develop new tools for stroke diagnosis, treatment, and recovery,” says Paul Rothman, the Frances Watt Baker, M.D., and Lenox D. Baker Jr., M.D., Dean of the Medical Faculty and CEO of Johns Hopkins Medicine. “These efforts will improve the health of millions of people in Baltimore, the UAE, and around the world.”
Facilitating Patient Access to Cancer Treatment

Sidney Kimmel Comprehensive Cancer Center patient Connie Veillette, PhD, first came to Johns Hopkins in early 2015 after having a reoccurrence of pancreatic cancer.
“When I received my initial diagnosis, I thought it was a death sentence,” Veillette remembers. “But this is something that I need to figure out and to fight.”
In spring 2018, Johns Hopkins opened a $100 million cancer center that combines treatment with research. Named for philanthropist and pancreatic cancer patient Albert P. “Skip” Viragh Jr., the Skip Viragh Outpatient Cancer Building aims to facilitate patient access to treatment by locating all cancer services in one place.
“The new Skip Viragh Building is a remarkable place because cancer patients have access to a whole range of services in that building. It’s only through this cross-disciplinary approach that you actually make breakthroughs,” Veillette says. “I’m still in the fight of my life, and I need to be at a place where I feel that people are in that fight with me.
“I have almost made it to five years,” she continues. “So I can say, ever so humbly, that I’m winning.”